When I first heard about the concept of an urgent care clinic for mental health, I thought it couldn’t work. What about the importance of the treatment relationship? Isn’t that the key to good clinical care? And besides, I had heard that the few urgent clinics that exist around the country have patients coming in and waiting 4 hours, or sometimes all day, just to be seen. Wouldn’t any mental health urgent care fill up, leaving the same access to care problems that existed before its inception?
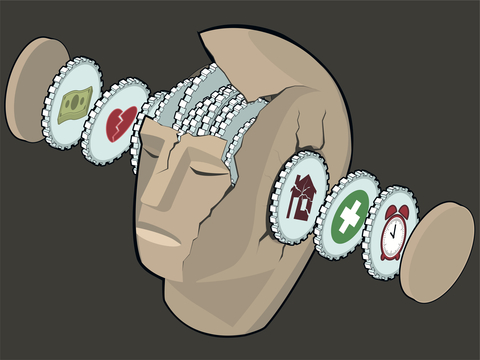
At the same time, access to psychiatric services is becoming more and more difficult. The typical scenario for people seeking mental health care services in my community progresses as follows:
1. An unexpected crisis hits, so the individual in crisis seeks care at an emergency room or medical urgent care. A doctor or PA assesses the patient and may recommend hospitalization, but usually not. (Mental health hospitals provide care for a few days when necessary for safety. If there is not a safety concern, hospitalization is usually not the best option). The doctor/PA perhaps prescribes a Xanax like medication (probably not the best treatment for he problem, but available in the ER) and recommends ongoing care with a psychiatrist, but doesn’t know anyone who is taking new patients.
2. The patient, hopefully stable enough to wait, calls around town and finds out very few psychiatrists accept her insurance, and many of those who do take her plan have full practices. She finally finds someone and schedules an appointment with psychiatrist’s office, but will have to wait 4 months for the initial evaluation.
3. Uncertain she can wait 4 months; she reluctantly goes to her primary care physician (to whom she had not wanted to disclose the psychiatric problem, because she felt ashamed). The PCP starts a medication, but both he and the patient feel uncertain that they understand the problem fully and both would prefer the opinion of a specialist, which they must wait 120 days to hear.
4. When she does finally meet with the psychiatrist, she finds that this person is not a good fit for her needs. He’s a specialist in PTSD and mostly treats veterans with medications only. He has 10-15 minute appointments. The patient is a 50-year-old woman with depression, and she wanted longer sessions with her doctor. 10 minutes is not enough time to get her concerns heard. She also preferred to see a female psychiatrist, but couldn’t find one who was taking new patients.
If, however, the patient above can seek care from a mental health urgent care center, the scenario can look quite different.
1. A crisis hits and the patient seeks care at a same day appointment. She is assessed by a team consisting of a therapist and psychiatrist, and a treatment plan is developed which includes both short term psychotherapy and starting an antidepressant. She may also be referred to a group for psychotherapy.
2. As part of the treatment plan, a long term strategy is developed for the patient’s continued care. Her choices for care include returning to primary care to maintain treatment once her symptoms are stable, having the mental health urgent care center facilitate an appropriate referral to a psychiatrist who provides the services she needs, or waiting on a waiting list with a community provider while the MHUC provides bridge care in the interim.
3. The MHUC stabilizes the patient, decreases emergency room and hospital utilization, and offers a screening process for the patient so she can land in the right place for care.
And what about the 4-hour wait times? I think the answer is that we need more than just a few of these specialized urgent care centers to provide the necessary services. The problem has been that only a few small clinics offered walk-in assessments for mental health. Many of these clinics were state funded, and had limited budgets. When the clinic budget was used up, the walk-in services began to clog up and drop in quality.
The answer will be to offer more options for walk-in care. To keep pace with the demand, the number of providers will have to increase over time. By returning patients to primary care when possible, using counseling professionals to fill in gaps, and focusing on the acute phase of treatment, I believe this can be achieved. Psychiatrists can offer consultation at the onset of an illness, and then allow other professionals to continue the plan later. Urgent care centers may be the best way to deliver specialty care in other fields as well (like orthopedics and internal medicine diagnostics), so that brief periods of consultation can then be followed by longer term follow-up in primary care.